Observation
Adapted posture due to pain might be present.
Observe the body morphology, as obesity may cause excessive load to the intervertebral discs, especially in the lower lumbar spine.
Examination
Physical examination should follow the anamnesis for a more accurate diagnosis (Kester et al. 2002).
Range of motion
There is pain in flexion (Magee 2006). Attention: the ROM findings may be due to normal age changes and not to the actual pathology (Foster et al 2012). The finger-floor distance should be measured, since an increased distance (esp. >25cm) is a significant predictor of nerve root compression (Kester et al. 2002).
Special Tests
-
Straight leg raising test (or Lasègue test)
-
Crossed straight leg raising test: The test is similar to the straight leg raising test, but the contralateral leg is raised passively and the sign is positive if sciatica is reproduced or exacerbated.
Other tests like the Bell’s test and the hyperextension test can be used as an adjucent to confirm the diagnosis. Sensitivities, specificities and positive predictive values (PPV) of bell test and hyperextension test are of interest. The combination of bell and hyperextension test has excellent specificity (0.92–0.94) and a good PPV (up to 0.85) for the diagnosis of disc herniation (Drapé 2001). More evidence on these tests is needed.
The slump test is the most common neurological test looking for increased tension in the neuromeningeal tract (Magee 2006). In the research of Majlesi et al (2008), the Slump test was found to be more sensitive than the SLR in the patients with lumbar disc herniations. However, the SLR was found to be a slightly more specific test than the Slump test. The straight leg raising test (SLR) and crossed straight leg raising test have both good positive predictive values for nerve root compression in herniated disc patients (Drapé et al. 2001). Combining positive test results increases the specificity of these physical tests (Aertgeerts et al. 2010). The SLR has a relatively high sensitivity (91%) but modest specificity (26%) for diagnosing herniated disc (Casey et al. 2007; Bezemer et al. 2000). The diagnostic accuracy of the straight leg raising test is limited by its low specificity (Bezemer et al. 2000). The crossed straight leg raising test is more specific (88%), but less sensitive (29%) than the SLR (Casey et al. 2007; Bezemer et al. 2000).
Neuromuscular
Magee (2006) states that myotomes are seldom affected, dermatomes not affected. According to Casey et al. (2007), back pain with leg pain in a typical lumbar (L4 L5 or S1) nerve root distribution is a key feature for the diagnose a herniated disc. These symptoms have a fairly high sensitivity but uncertain specificity. Knee strength and reflexes (L4), great toe and foot dorsiflexion strength (L5), foot plantar flexion and ankle reflexes (S1) should be tested, as well as the distribution of sensory symptoms to assess the presence and severity of nerve root dysfunction (Casey et al. 2007). Kester et al. (2002) associate typical dermatomal pain, paresis and absence of knee or ankle tendon reflex to nerve root impingement, especially the paresis is said to be a significant predictor. (Foster 2012). differentiates between two types of herniations, one associated with neural compression, therefore causing all the symptoms. The other type is due to neural toxicity, which leads to irritation (radiating pain) but not to actual compression (Foster 2012).
Myotome, dermatome and reflex testing should be performed, although not finding an impairment does not conclude there is no herniation. When you find weakness in a dermatome, suspect impingement of the corresponding motor nerve, finding numbness suggest compression of a sensory nerve and radicular pain is due to inflammation or irritation of the nerve (Foster 2012). The typical dermatomal pain distribution is reported to have a high sensitivity, 90% in the study of Kester et al. (2002), 99% in the study of Kerr et al. (1988).
Diagnostic imaging
After one month of symptom onset, one should perform a MRI and eventually consider EMG and/or NCV (Casey et al. 2007). MRI is reported to be the first choice to diagnose a disc herniation (Milette 2000). According to Kester et al (2002) sensitivity and specificity values of MR imaging in the diagnosis of disc herniation range from 71% to 100% and from 50% to 86%. Nevertheless, the association of the imaging findings and the patient’s symptoms is weak. Quite often, imaging diagnostic tests show herniated discs belonging to a-symptomatic patients.
Differential diagnosis
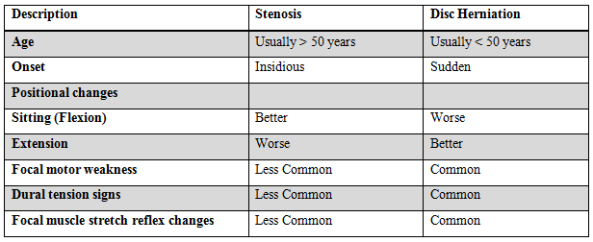
Comparison of spinal stenosis with disc herniation (Thomas 2003)
It is important to exclude cauda equina syndrome, spinal fracture, cancer or infection of the spine, pyriformis syndrome, and nerve entrapment at the fibular head. Also differentiate disc herniation from referred pain coming from the hip, sacroiliac joint, intervertebral joints, or painful muscles (trigger points) or tendons.
k